Aggravated Disc vs Herniated Disc: What's the Difference and When Should You See a Physio?
"I've done something to my disc." Physios hear this all the time. The person has lifted a box, woken up crooked, or gradually seized up after weeks at their desk. Then they start googling and find themselves sorting through a lot of medical terminology. Herniated disc. Bulging disc. Slipped disc. Prolapsed disc. Disc protrusion. Aggravated disc.
This guide will help you understand the differences between these terms, what causes each type of disc problem, and when to seek treatment.
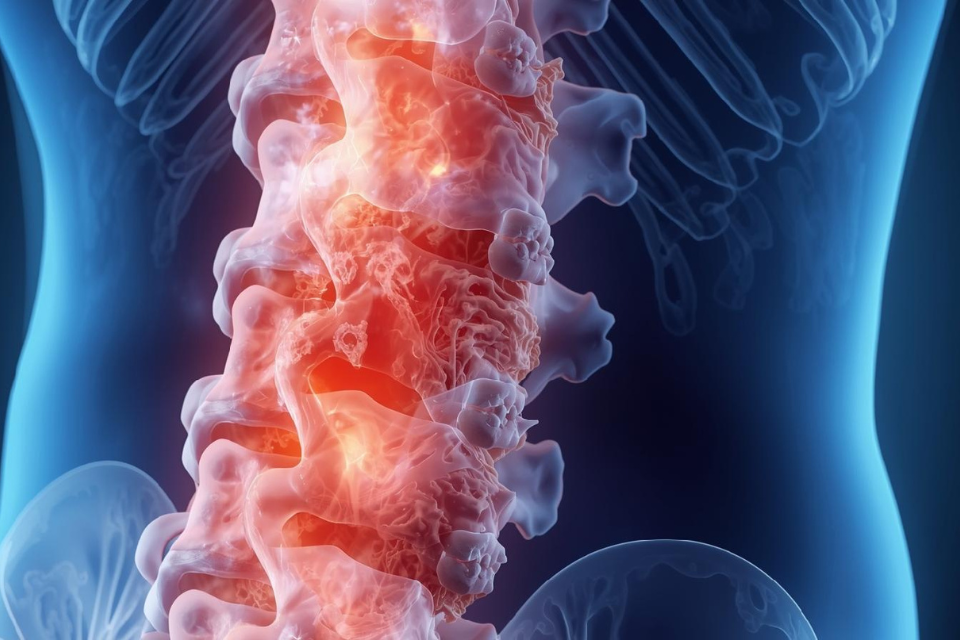
Spinal Disc Anatomy
Your spine has 24 vertebrae that can move, and between each pair sits a disc. These discs are basically shock absorbers, taking the load when you walk, bend, twist or run.
Inside each disc there are two parts. The middle bit is called the nucleus pulposus, which is soft and gel-like with a high water content (around 80%). Wrapped around that is the annulus fibrosus, a tougher outer ring made up of collagen fibres. There are somewhere between 15 and 20 layers of these fibres, depending on which research you look at.
The jam doughnut comparison gets used a lot. Soft filling in the middle, firmer casing on the outside. It's a decent enough analogy. The trouble starts when that outer casing gets damaged.
Aggravated Disc
Aggravated disc isn't a formal diagnosis you'd find in a medical textbook. It's more of a descriptive term for when a disc is irritated or inflamed but hasn't actually bulged or herniated yet.
How does someone aggravate a disc?
It could be from lifting something heavy with a rounded back, spending too long hunched at a desk, or sometimes an old disc injury just flares up again without any obvious trigger. Aggravated disc symptoms after lifting are pretty common, particularly after helping someone move house or shifting furniture.
What's actually happening in there?
Could be a few things. Inflammation building up around the disc. Tiny tears forming in those outer fibres. Maybe the early stages of a bulge developing. Often it's a mix of all three.
Symptoms are usually a deep ache in the lower back. Sitting for long periods makes it worse, so does bending forward. Mornings tend to be rough, and you end up constantly fidgeting trying to find a position that doesn't hurt. A lot of people find that walking around actually feels better than staying seated.
With the appropriate management, these symptoms may settle over time, though the timeline varies a lot from person to person. Physio for an aggravated disc generally focuses on what's driving it. The inflammation, any stiffness in the joints, and figuring out what activities keep setting it off.
Bulging Disc
With a bulging disc, the outer wall of the disc has weakened and is pushing outward beyond where it should be. Nothing has actually ruptured though, and the outer layer is still in one piece.
It's a bit like when a car tyre develops a bulge in the sidewall. The tyre hasn't blown out, but something's not right with the structure.
The bulging typically affects somewhere between a quarter and half of the disc's circumference. The gel centre stays contained inside, pressing against the outer wall but not through it.
What catches people off guard is just how common bulging discs are. If you scanned the spines of a hundred people over 40, many would show some bulging or degeneration. Many of them have no pain at all and never even knew there was a problem. You can walk around with a bulging disc for years without any symptoms.
When symptoms do occur, it's typically local pain in the back or neck along with some stiffness. The pain might spread into the buttocks or shoulders, and it tends to fluctuate with good days and bad days.
Can a bulging disc heal?
Symptoms do resolve in some cases as the body adapts and inflammation settles. How long this takes, and whether it happens at all, varies enormously between individuals.
Herniated Disc
A herniated disc is where actual structural failure has occurred. The outer wall has cracked or torn, and gel from inside has squeezed through. Other names for the same thing include ruptured disc, slipped disc, and prolapsed disc.
The reason this matters is that escaped disc material can now press directly on nerves. This nerve compression triggers chemical irritation and inflammation, and in severe cases it can involve compression of the spinal cord itself.
The symptoms tend to be more intense than with a bulge, and more specific too. Sharp shooting pain down an arm or leg, pins and needles, numbness, and actual weakness in muscles rather than just pain. Bending and twisting often make it worse. Doctors call this pattern radiculopathy, which basically means the nerve root is being irritated.
Sciatica is the well-known version, which is when a lumbar herniation affects the sciatic nerve. The pain travels from the back, through the buttock, and down the leg, sometimes right to the foot. It's one of the most common reasons people seek physiotherapy for back-related problems.
L4-L5 and L5-S1 are the spinal levels most frequently involved. The lower lumbar spine takes the most load, which is why back pain with leg symptoms is such a common combination.
The Key Difference Between a Bulging Disc and Herniated Disc
Bulging disc: the outer wall is weakened and pushing outward, but still intact. Contents remain inside.
Herniated disc: the outer wall has torn open. Contents have escaped.
A bulge can become a herniation over time if the weakened wall eventually gives way, but this isn't inevitable. Plenty of bulging discs stay stable for years. The reverse also happens, where some herniations improve on their own as the body gradually reabsorbs the escaped material.
When it comes to symptoms, bulges tend toward localised, achy pain while herniations more commonly produce that shooting nerve pain along with numbness, tingling, and weakness.
For those wondering about bulging vs herniated on MRI, imaging can typically distinguish between them. A bulge shows the disc pushing out fairly evenly, while a herniation shows a focal area where material has broken through.
Annular Tears
Annular tears often come before bulges and herniations. An annular tear is a rip in the outer fibres of the disc, usually small at first.
Different types exist depending on where the tear starts. Some begin from the inner layers and work outward, others start at the outer edge, and some run in circles around the disc. The direction can matter for prognosis.
The tricky part is that many annular tears cause no symptoms at all. The inner portion of the disc has few nerve endings, so pain receptors are sparse there. But the outer third is well-innervated, and once a tear reaches that zone it can hurt significantly.
The pattern is typically deep aching back pain that's worse with sitting and bending forward.
Healing is slow because the disc has poor blood supply. Timeframes of 18 months to two years are not unusual for full tissue healing. Physiotherapy is often used early to manage symptoms and address contributing factors while the slow healing process continues.
Getting a Diagnosis
A good clinical assessment can often identify the likely cause of back pain. History taking covers how it started, what makes it worse, and what helps. Physical examination looks at movement, strength, reflexes, and nerve function, and there are specific tests for identifying nerve involvement.
When does imaging make sense? If symptoms aren't improving after 6 to 8 weeks of treatment, if there are neurological symptoms like progressive weakness or bladder changes, or if there's concern about something more serious.
When an MRI for disc injury is needed, it's usually to confirm what the clinical picture already suggests or to clarify things before deciding on next steps. MRI shows soft tissue well and can identify bulges, herniations, and annular tears. X-rays and CT scans have other uses but aren't as good for disc problems specifically.
When to See a Physio
If you're experiencing back pain with any of the symptoms described above, it's worth speaking to a health professional to get a proper assessment. Physiotherapy is one option that may be helpful for some people, though the right approach varies depending on individual circumstances and should be determined through proper clinical assessment.
It's worth noting that conservative treatment (which includes physiotherapy) is generally considered as an initial approach for disc-related symptoms in people who don't have serious neurological deficits. However, this doesn't mean physiotherapy is appropriate for everyone, and outcomes vary significantly between individuals.
Some situations need urgent medical attention rather than physiotherapy. If you've got severe leg weakness that's getting worse quickly, numbness around your inner thighs, buttocks or genitals (the saddle area), or any changes to your bladder or bowel control, see a doctor immediately. Same with any major trauma to your spine. These symptoms could indicate cauda equina syndrome, which is rare but requires emergency treatment.
What Happens During a Physiotherapy Treatment
There's no single protocol that fits everyone, so treatment gets tailored to what's actually going on.
Hands-on treatment features in most disc management. Mobilisations help with stiff segments, though physios tend to avoid high-velocity manipulation with acute disc problems due to the potential to aggravate things.
Muscle work often forms part of treatment too. When there's a disc problem, the surrounding muscles tend to seize up as a protective response. It's understandable, but it adds to the pain. Massage, trigger point work, and dry needling are sometimes used to address this guarding as part of a broader treatment plan.
Exercise sits at the centre of most treatment plans and usually involves strengthening the deep core muscles, improving mobility where it's lacking, and addressing any strength imbalances that may have contributed to the problem.
Education matters as well. Understanding what's happening, which movements to back off temporarily, how to set up a workstation, and how to manage flare-ups if they occur all play a role.
Traction is sometimes included with the aim of reducing pressure on the affected disc. This can be done manually or with equipment.
Recovery Times
Everyone asks about herniated disc recovery time, which is understandable, but precise timeframes are difficult to give because there are so many individual factors at play.
As a rough guide, straightforward aggravated discs or minor bulges may improve within a few weeks for some people. More significant bulges or smaller herniations may take longer, potentially several months.
Larger herniations are a longer road. The body can reabsorb herniated material over time, but the speed varies enormously between individuals.
Annular tears tend to be the slowest due to the limited blood supply to the disc. Full tissue repair can take over a year in some cases, though symptom improvement often comes earlier.
Treatment is adjusted as things progress, since what's appropriate early on differs from what's needed later in recovery.
Looking After Your Spine
Some disc degeneration is unavoidable because discs wear down with age. But there's plenty that can be done to reduce risk.
Movement is probably the biggest factor. Discs need movement to stay healthy as it's how they receive nutrients and clear waste. Walking, swimming, and cycling all work well, and nothing extreme is required.
Core strength matters too. Strong deep muscles can reduce load on the discs, and basic exercises done consistently are often included in management plans.
Posture is worth paying attention to, particularly for desk workers. Slouching loads the discs significantly more than sitting upright, and regular breaks from the computer help.
Lifting technique counts as well. Bend your knees, keep the load close to your body, and avoid twisting at the same time. Get help with heavy items.
Weight plays a role for lower back discs specifically. Extra kilos around the middle means extra compression on the lumbar spine.
Smoking affects discs too by reducing blood flow and accelerating degeneration. It's not an obvious connection but it's a real one.
Disc Treatment in Adelaide
If you're dealing with back pain that might be disc-related, a physiotherapy assessment may help identify what's contributing and guide appropriate management.
Ducker Physio has two Adelaide clinics offering assessment and treatment for disc-related conditions: Magill on The Parade and Salisbury on Mary Street. Ducker Physio is also the physiotherapy provider at Calvary Central Districts Hospital in Elizabeth Vale.
No GP referral is needed. Same-day appointments are sometimes available and after-hours sessions are offered. For anyone unsure whether physio is the right fit, initial 20-minute assessments are available to talk through symptoms and options.
Ducker Physio Magill 465/467 The Parade, Magill SA 5072 Phone: 08 7092 5962
Ducker Physio Salisbury 9 Mary Street, Salisbury SA 5108 Phone: 08 7092 5964
This is general information only and does not substitute for assessment by a health professional familiar with your specific situation. Severe symptoms, worsening weakness, or changes to bladder or bowel function require urgent medical attention.
Frequently Asked Questions
-
The main signs include sharp shooting pain that travels down an arm or leg, pins and needles, numbness, and muscle weakness. The pain typically gets worse with bending or twisting. If the herniation is in the lower back and affecting the sciatic nerve, you might feel pain running from your back through your buttock and down your leg.
-
Recovery time varies significantly between individuals and depends on the size and location of the herniation, as well as other factors. Some people notice improvement within a few weeks, while others may take several months. The body can gradually reabsorb herniated disc material over time, though this process is unpredictable.
-
Ducker Physio has two clinics offering assessment and treatment for disc-related conditions. If you're looking for bulging disc treatment in Magill or sciatica physio in Salisbury, both clinics provide the same services for herniated discs, bulging discs, sciatica and other spinal conditions.
-
Not always. A thorough clinical assessment can often identify the likely cause of back pain without imaging. MRI may be recommended if symptoms aren't improving after 6 to 8 weeks of treatment, if there are significant neurological symptoms, or if there's concern about something more serious.
Sources
https://www.ncbi.nlm.nih.gov/books/NBK459235/
https://www.ncbi.nlm.nih.gov/books/NBK560878/
https://www.ncbi.nlm.nih.gov/books/NBK542307/
https://www.ncbi.nlm.nih.gov/books/NBK535373/
https://pmc.ncbi.nlm.nih.gov/articles/PMC10882128/
https://link.springer.com/article/10.1007/s00586-010-1603-7